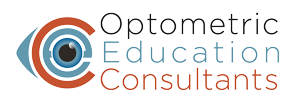
A 65 year old woman previously diagnosed with primary open angle glaucoma presented for ongoing care. She was using latanoprost in each eye and had bilateral selective laser trabeculoplasty performed two years earlier. Her medical history was significant for hypertension, elevated cholesterol, and arthritis. Her vision was 20/20 OD and 20/25 OS. She had an inferior retinal nerve fiber layer defect in the right eye and significant superior rim damage in the left eye. Threshold perimetry showed the above corresponding visual field defects.
However, there was no anatomical correlate to explain the inferior defect in the right eye. Particularly troubling was the fact that on the Greyscale, the inferior defect on the right eye broke from the blind spot and stopped at the vertical. Upon inspecting the left inferior arcuate defect, it was seen that there was a deeper scotoma underlying inferior nasally, also seemingly stopping at the vertical. It appeared that there was a right inferior quadrantanopia underlying the glaucomatous fields. Threshold perimetry was repeated and these patterns persisted. She was referred for neuroimaging. Interestingly, while awaiting the MRI results, the patient called in to report that she remembered a transient period of inability to speak 8 years earlier that had been attributed to a “mini-stroke”. MRI revealed past ischemic changes and the patient’s internist is intervening to attempt to prevent future cerebrovascular events.
This case underscores the importance of recognizing potential neurogenic fields which may be lost among glaucomatous vision loss. While historically disregarded, remember that the Greyscale on the visual field does impart valuable information.