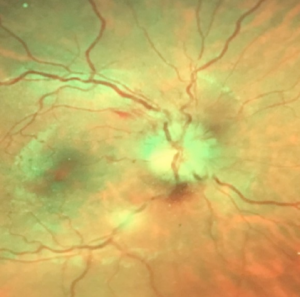
Case 1: A 27 year old woman presents urgently complaining of painful vision loss in her right eye. She has no known medical history and this has never occurred before. She has an edematous optic nerve with hemorrhaging, an afferent pupil defect, superior arcuate scotoma, pain when she moves her eye, and 20/70 visual acuity. A clear-cut case of optic neuritis possibly as the first manifestation of multiple sclerosis? Perhaps…perhaps not.
While it is tempting to look at an acute optic neuropathy with pain on eye movement in a young female and immediately surmise optic neuritis and a possible demyelinating disease such as multiple sclerosis, there are inconsistencies which must be considered. Demyelinating optic neuritis presents with a normal optic disc in the majority of cases. Additionally, disc and juxtapapillary hemorrhages are extremely rare in optic neuritis, so other causes must be considered.
Non-arteritis anterior ischemic optic neuropathy (NAAION) can have a similar optic disc appearance. NAAION will typically have inferior visual field defects. More importantly, NAAION is a painless condition. Arteritic anterior ischemic optic neuropathy would not be considered because of the patient’s age.
Infectious optic neuropathy needs to be strongly investigated in a case like this. Neuroretinitis, often associated with cat-scratch disease, will present with a macular star of exudates, but this finding may be missing early in the disease. However, optical coherence tomography (OCT) will show a serous macular detachment early in the disease course.
In this case, contrast-enhanced MRI of the orbits/chiasm and brain should be ordered to rule out demyelination and neural sheath swelling in perineuritis. Macular OCT should be performed to look for a serous detachment suggestive of neuroretinitis. The patient should also be tested for numerous infectious agents including Bartonella, syphilis, Lyme, tuberculosis, herpes, Epstein-Barr, and rickettsioses, to name a few. This can best be done in concert with the patient’s primary care physician or an infectious disease specialist.
MRI findings showed optic nerve enhancement possibly consistent with infectious, autoimmune, or granulomatous disease with no evidence of demyelination. Serological testing subsequently revealed very high titers of Epstein Barr Nuclear Antibody IgG and Epstein Barr Capsid Antibody IgG.
The pathogenesis of infectious optic neuropathies may involve direct involvement of the optic nerve by a pathogen and /or indirect involvement with inflammatory, degenerative, or vascular mechanisms.
Thanks to Dr. Nikki Rook for sharing this case